Nitish Boodhoo, University of Guelph
The confirmed presence of bird flu in American dairy cattle in a March 25 report from the U.S. Department of Agriculture (USDA) — and a case in Texas where a human working with cattle was infected — has put Canadian public health experts on high alert.
But, what is bird flu and what do we know about influenza in both poultry and cattle?
Bird flu, also called avian flu, refers to infection caused by the avian influenza Type A viruses. In the wild, influenza viruses generally spread among migratory waterfowls, such as ducks and geese. Within avian species, domestic poultry are highly susceptible to infection with Type A avian influenza viruses, including H5N1.
Canada itself is amid an H5N1 avian influenza virus outbreak, with over 11 million domestic poultry estimated to be affected and culled to date. In fact, a major concern for the Canadian poultry supply chain is the incurred financial loss from culling birds.
This virus is highly contagious among domestic poultry and can spread through an entire flock within a matter of days. The most common route of transmission from an infected bird to a non-vaccinated bird is via direct physical contact or contact with virus-contaminated surfaces with bodily fluids such as oral mucus and feces.
Bird flu in mammals
Non-avian species, like mammals, can also become infected with the H5N1 virus. In Canada, sporadic cases of mammals becoming infected with bird flu have been reported in raccoons, striped skunks, red foxes, cats and dogs.
As of March 2024, various reports from the USDA, Food and Drug Administration, and Centers for Disease Control and Prevention (CDC) confirmed the presence of H5N1 in dairy cattle across eight states, of which Idaho, Ohio and Michigan are the most northern states bordering Canada.
Although there are no known reports indicating the current bovine strain has made its way into Canada, there is no doubt that it is getting too close for comfort. As of March 27, 2024, the Canadian Food Inspection Agency has established various primary control zones in Alberta to prevent the spread of H5N1.
The emerging bovine H5N1 virus is novel to the cattle industry, a backbone of the Canadian food and agriculture industry. The close environmental relationship between humans and cattle would seem to make both species more vulnerable to influenza transmission, but that is not the case.
Interestingly, only a few cases of cattle-to-human influenza transmission have been documented. In contrast, pigs are the main mixing vessel for avian influenza A viruses, as exemplified in the 2009 H1N1 swine flu pandemic. The 2009 swine H1N1 virus was a mixing event that led to mammalian adaptation, a process that is not straightforward in any intermediate host. A natural mixing event in pigs would result from exchange of genetic material following co-infection with both an avian and human influenza virus.
However, in the current scenario, the emerging bovine H5N1 strain that has infected American dairy cattle has undergone a specific adaptation in an enzyme called polymerase. Changes to this viral enzyme are concerning, as it could allow for faster adaptation and maybe even support cattle-to-cattle transmission.
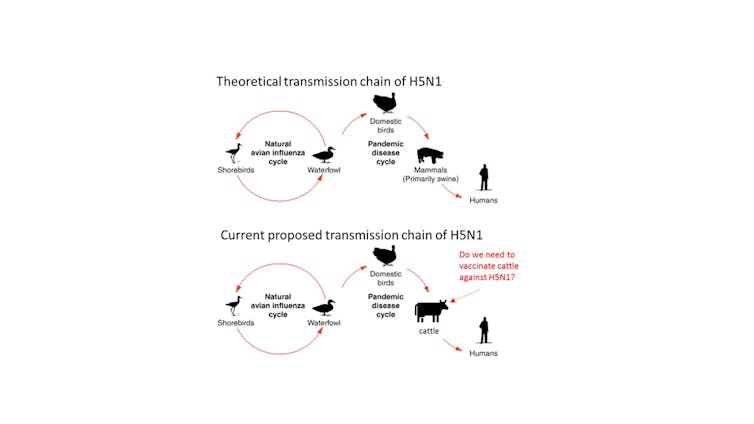
(Nitish Boodhoo)
This raises numerous questions for which the answers are not yet clear. Among these, the key questions are:
- How are dairy cattle getting infected?
- Is viral transmission from infected to non-infected cattle, or strictly direct contact with contaminated surfaces or infected birds?
- Are cattle relevant as an intermediary in the transmission chain of Type A influenza viruses such as H5N1 from poultry to cattle, eventually infecting humans?
The answers will support new regulations to control H5N1 spread within dairy cattle and to other farms, poultry, mammals and humans. The greater concern would be if this virus has entered the pig industry.
Are there vaccines against H5N1 for humans and livestock?
According to a CDC report, the H5N1 viral strain that infected a human in Texas is closely related to two candidate vaccines. It is also reassuring to know that the World Health Organization maintains a list of candidate vaccines that could be mass-produced against H5N1 influenza viruses. In fact, some countries maintain a small stockpile of vaccine doses against H5N1, should there be a need to vaccinate at-risk populations.
Until such an outbreak event occurs where vaccines against H5N1 for people might be required, the Canadian government has a list of preventive measures that people can take.
Members of the public need to keep their distance and avoid direct contact with wild birds that look sick or have died. People should also avoid touching surfaces where there are likely to be bird droppings.
As for livestock species, both the American and Canadian governments have been reluctant to approve the use of vaccines in the poultry industry. The long-standing strategy against avian influenza has been eradication, and not vaccination, by culling all infected and affected chickens. While it has been successful at preventing the virus from becoming endemic, it may not be economically sustainable with H5N1 outbreaks predicted to occur on a yearly basis.
In the wake of this unprecedented news, efforts have to be directed to study avian influenza transmission from poultry into cattle. Such proactive efforts will hopefully generate necessary data to establish a decision-making framework to safeguard our livestock industry and protect human health.![]()
Nitish Boodhoo, Research Associate, Department of Pathobiology, University of Guelph
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Relevant Agribook pages include “Animal husbandry” and “Biosecurity“.
Photo by Jan Koetsier: www.pexels.com/photo/black-and-white-dairy-cow-s-head-2647053/
